Issue 2: Beyond Keto: The Real Science of Insulin Resistance
How ketones condition Macrophages
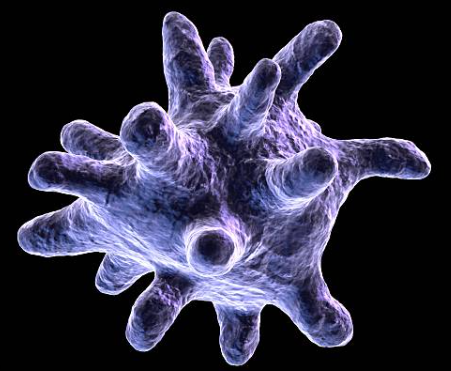
Macrophages are programmable. In broad strokes, M1 macrophages amplify inflammation and microbe-killing, while M2 macrophages resolve inflammation and repair tissue.***
Ketone bodies—especially β-hydroxybutyrate (BHB)—nudge that balance by changing signals, enzymes, and even epigenetics inside these cells.
***This is a very broad generalization and not the way I like to think of macrophages but it’s a common way to talk about them without going into the complexities of macrophage profiles. For an overview of macrophages, you can watch my presentation at IHMC for a lay audience: https://youtu.be/-CQqfkrae00?si=Lkuqlyi18NamHaLg
1) Inflammasome brake: BHB → ↓ NLRP3
BHB directly blocks the NLRP3 inflammasome, the molecular “match” that ignites IL-1β and IL-18 release in M1 states. Mechanistically, BHB prevents K⁺ efflux and ASC speck formation, damping the cascade without needing AMPK, ROS, or autophagy pathways. In mice, raising BHB levels reduced NLRP3-driven inflammatory disease.
Why it matters: turning down NLRP3 lowers a key amplifier of sterile inflammation (metabolic syndrome, neuroinflammation, gout), biasing macrophages away from an M1 phenotype. Additional work extends this effect to neutrophils and brain inflammation models.
2) Receptor signal: BHB → HCAR2 (GPR109A)
BHB is also a ligand for HCAR2 (GPR109A), the same receptor hit by niacin and dimethyl fumarate. Activating HCAR2 on monocytes/macrophages promotes an anti-inflammatory program and, in neuroinflammatory models, was necessary for the protective effect of ketogenic states. Recent structural/biased-agonism studies strengthen the case that HCAR2 signaling in macrophages is a druggable anti-inflammatory axis.
3) Epigenetic tune-up: BHB as an HDAC inhibitor
Inside cells, BHB acts as an endogenous class I HDAC inhibitor, increasing histone acetylation and stress-resilience gene expression. That epigenetic shift supports a tilt away from pro-inflammatory transcriptional programs—one reason fasting/ketosis often correlates with a calmer innate immune tone.
4) Polarization programs: toward M2, away from M1
Beyond blocking NLRP3, BHB promotes M2-like features via STAT6-dependent signaling in colitis models (more repair, less tissue damage). Newer work shows BHB can post-translationally modify key proteins (lysine β-hydroxybutyrylation), including STAT1, blunting its LPS-driven M1 transcription—another route away from inflammatory polarization.
Functional upshot: in spinal cord injury and other contexts, ketogenic metabolism correlated with more M2 markers, less inflammatory damage, and better tissue recovery—consistent with the mechanistic signals above. (Animal/early translational evidence; human confirmation needed.)
5) Important nuance (read this***)
- Context matters. Substrate mix, glucose availability, species, and tissue niche shape outcomes. One livestock study showed low glucose + BHB could increase pro-inflammatory signaling via GPR109A/NF-κB in yak alveolar macrophages—useful as a reminder that biology isn’t one-note. PubMed
- Endogenous vs exogenous. Nutritional ketosis changes many levers at once (substrates, hormones, redox, gut signals). A ketone drink spikes BHB for hours but doesn’t recreate the full milieu; immune effects may therefore differ in size or direction. (Inference built on mechanistic and clinical contrasts from this issue.)
- Dose & duration. Many immune effects were shown at millimolar BHB and over short windows; long-term human data on macrophage polarization with therapeutic ketosis are limited.
Ketones don’t just fuel cells; they condition them. In macrophages, BHB dampens a core inflammatory switch (NLRP3), signals through HCAR2 to reduce inflammatory tone, and rewrites gene programs via HDAC inhibition and β-hydroxybutyrylation—changes that, together, bias toward M2-like, pro-resolution behavior. It’s elegant biology with clinical promise, worth watching, but not yet a license for supplement hype.
References
- Youm YH, et al. “BHB blocks NLRP3 inflammasome.” Nat Med. 2015.
- Rahman M, et al. “HCAR2 activation in monocytes/macrophages.” Sci Rep. 2022
- Taggart AK, et al. “GPR109A in inflammation.” Nat Med. 2005.
- Shimazu T, et al. “BHB as an endogenous HDAC inhibitor.” Science. 2013.
- 5. Xie Z, et al. “Lysine β-hydroxybutyrylation and metabolic signals.” Cell Metab. 2016.
- Rahman M, et al. “BHB modulates macrophage phenotype.” J Neuroinflammation. 2014.
- Tan M, et al. “Ketogenic metabolism and macrophage M2 polarization.” Front Immunol. 2022.
- Wang T, et al. “Low-glucose + BHB induce macrophage inflammatory signals in yak lung models.” Front Vet Sci. 2022.
Need the bottom line on insulin resistance? Read Postscript next and get the heads-up on your upcoming weekly action lists.
Explore more from Issue #: Beyond Keto: The Real Science of Insulin Resistance
Pick the next section to read in Issue #1
